MEDICAL REFRACTORY EPILEPSY
Remote patient diagnosis & consultation
To simplify the initial contact with our hospital for patients from abroad, we have prepared a remote two-stage process of prequalification for neurosurgical procedure. In the first stage, the patient sends via email all available medical documentation (lab results, treatment history, MRI scans) to be analyzed by our neurosurgical team. In second stage, we will arrange an on-line video consultation with one of our neurosurgeons. The cost of the online consultation is 200EUR. All necessary exams (e.g. CT, MR) and consultations will be repeated during the patient’s stay at Vital Medic Hospital. The final therapeutic decision will be based on neurosurgical exam and radiological results. At this point the final financial settlement may be presented to the patient. The neurosurgical treatment will be carried out according to the schedule determined by the team of specialists. We encourage you to use the email below or the contact form to begin your treatment.
Comprehensive and coordinated treatment
Comprehensive and coordinated treatment for brain and spine tumors takes place at the Brain and Spine Tumor Treatment Center, where we provide:
• Neurosurgical/neurological consultations – initial, to diagnose the disease
• Diagnostic tests appropriate for the initial diagnosis
• Qualification for surgical treatment
• Individually selected surgery with the use of advanced technology for planning and performing the procedure
• Individually planned perioperative and postoperative neurological rehabilitation
• Follow-up consultations for post-op control and continuation of the treatment
PROCEDURES
VNS, vagus nerve stimulation
The procedure involves implanting a generator and vagus nerve stimulation electrodes under the skin. The procedure is performed without age restrictions. The antiepileptic mechanism of vagus nerve stimulation is not fully understood. The effect of stimulation of vagus nerve structures (myelinated and nonmyelinated fibers) is believed to be directly on the nucleus of the solitary band, and from there toward the limbic system and the insula.

VNS SenTiva Stimulator
SenTiva is an implantable and programmable pulse generator for the treatment of refractory epilepsy. It provides stimulation that responds to the rapid increase in heart rate that can be associated with seizures, allows day-night programming, schedule programming, and logging of low heart rate events and abdominal position.
DBS, deep brain stimulation
A novel method, it involves stereotactic implantation bilaterally into the deep structures of the brain of a small electrode connected to a stimulator placed under the skin or pectoral muscle. The stimulators record a recording of the brain’s bioelectrical activity and respond only if abnormal discharges occur. During DBS, stimulation can target one or multiple epileptic foci. Stimulation of the deep nuclei results in secondary diffuse stimulation of extensive cortical areas by taking advantage of the many pathways and connections that exist between deep structures and areas of the cortex.
For neurostimulation of deep brain structures, we use Boston Scientific’s Vercise Genus rechargeable stimulator:
The Vercise Genus R16 stimulator is equipped with Cartesia 3D technology, a set of programming features that provide targeted therapy with less risk of side effects. It also makes it easier for the doctor to adjust and fine-tune the stimulation over time, so the patient can be sure to continue receiving the therapy they need. Because the battery can be recharged wirelessly for at least 15 years, several non-rechargeable pacemaker replacement procedures can be avoided during that time.
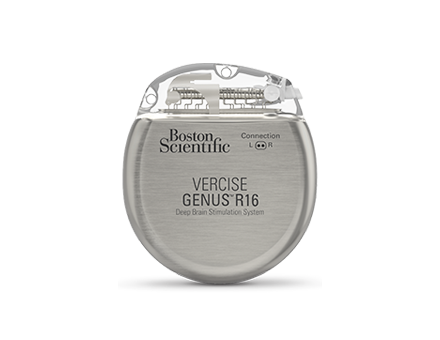
Features of the stimulator:
– Light weight and size of the device, the patient experiences less discomfort after implantation
– Battery life of at least 15 years, covered by warranty
– Wireless battery charging
– Bluetooth wireless remote control
– MR examination capability
– Constant-current stimulators
– With Cartesia 3D technology, Vercise DBS electrodes allow independent control and precise adjustment of stimulation size and shape, accurately targeting therapy and avoiding unwanted side effects
As part of the lobectomy procedure, the part of the lobe of the brain that is responsible for generating epileptic seizures is removed. Most often, the medial structures of the temporal lobe are removed (amygdalohippocampectomy).
Intraoperative Neuromonitoring
Intraoperative neuromonitoring is a diagnostic tool that is used during surgery. This method is based on the fact that nerve impulses are in the form of microelectric impulses which can be detected with super-sensitive equipment. During surgery, impulses are detected and recorded from the cortex of the brain responsible for example for hand movement. This method is also used for intraoperative mapping of eloquent structures for example visual or speech cortex. In that case direct electrical stimulation is used to induce neurological effects (speech arrest, visual disturbances, etc.) during awake craniotomy. This method allows to increase safety and improves neurological outcome of neurosurgical procedures. Intraoperative neuromonitoring performed during deep brain stimulation surgery is necessary for correct electrode placement by the neurosurgeon.
Lesionectomy surgery focuses on removing an isolated lesion (such as a tumor or malformed blood vessel) that is responsible for epileptic seizures.
Intraoperative Neuromonitoring
Intraoperative neuromonitoring is a diagnostic tool that is used during surgery. This method is based on the fact that nerve impulses are in the form of microelectric impulses which can be detected with super-sensitive equipment. During surgery, impulses are detected and recorded from the cortex of the brain responsible for example for hand movement. This method is also used for intraoperative mapping of eloquent structures for example visual or speech cortex. In that case direct electrical stimulation is used to induce neurological effects (speech arrest, visual disturbances, etc.) during awake craniotomy. This method allows to increase safety and improves neurological outcome of neurosurgical procedures. Intraoperative neuromonitoring performed during deep brain stimulation surgery is necessary for correct electrode placement by the neurosurgeon.
The corpus callosum is a set of nerve fibers connecting the two halves of the brain. Cutting the fibers – a calozotomy is an operation in which all or part of this structure is cut, resulting in a lack of communication between the hemispheres and preventing seizures from spreading from one side of the brain to the other. The procedure is called a disconnection.
Intraoperative Neuromonitoring
Intraoperative neuromonitoring is a diagnostic tool that is used during surgery. This method is based on the fact that nerve impulses are in the form of microelectric impulses which can be detected with super-sensitive equipment. During surgery, impulses are detected and recorded from the cortex of the brain responsible for example for hand movement. This method is also used for intraoperative mapping of eloquent structures for example visual or speech cortex. In that case direct electrical stimulation is used to induce neurological effects (speech arrest, visual disturbances, etc.) during awake craniotomy. This method allows to increase safety and improves neurological outcome of neurosurgical procedures. Intraoperative neuromonitoring performed during deep brain stimulation surgery is necessary for correct electrode placement by the neurosurgeon.
It is a type of hemispherectomy, a procedure that involves the resection of one hemisphere of the brain. Functional hemispherectomy is the separation of one hemisphere from the other and removal of a small part of the brain. It is used in situations where the entire hemisphere is not working properly.
Intraoperative Neuromonitoring
Intraoperative neuromonitoring is a diagnostic tool that is used during surgery. This method is based on the fact that nerve impulses are in the form of microelectric impulses which can be detected with super-sensitive equipment. During surgery, impulses are detected and recorded from the cortex of the brain responsible for example for hand movement. This method is also used for intraoperative mapping of eloquent structures for example visual or speech cortex. In that case direct electrical stimulation is used to induce neurological effects (speech arrest, visual disturbances, etc.) during awake craniotomy. This method allows to increase safety and improves neurological outcome of neurosurgical procedures. Intraoperative neuromonitoring performed during deep brain stimulation surgery is necessary for correct electrode placement by the neurosurgeon.
Morell’s procedure is used when epilepsy originates in areas that cannot be removed. The surgeon makes a series of incisions that interrupt the course of seizure impulses, but do not damage the brain.
Intraoperative Neuromonitoring
Intraoperative neuromonitoring is a diagnostic tool that is used during surgery. This method is based on the fact that nerve impulses are in the form of microelectric impulses which can be detected with super-sensitive equipment. During surgery, impulses are detected and recorded from the cortex of the brain responsible for example for hand movement. This method is also used for intraoperative mapping of eloquent structures for example visual or speech cortex. In that case direct electrical stimulation is used to induce neurological effects (speech arrest, visual disturbances, etc.) during awake craniotomy. This method allows to increase safety and improves neurological outcome of neurosurgical procedures. Intraoperative neuromonitoring performed during deep brain stimulation surgery is necessary for correct electrode placement by the neurosurgeon.
NEUROSURGERY DEPARTMENT
CONTACT
Vital Medic
46-200 Kluczbork
Skłodowskiej-Curie st. 21
Poland, opolskie region
Contact to our patient service:
📱 +48 531 999 172
📱 +48 531 439 671
✉ neuro@vitalmedic.pl
MAIN EMAIL
PATIENT COORDINATOR
Paweł Respondek
📞 +48 531 999 172
✉ p.respondek@vitalmedic.pl
PATIENT CARER
Nicoletta Nicowska
📞 +48 531 439 671
✉ n.nicowska@vitalmedic.pl
LEAVE US MESSAGE
WE WILL GET BACK TO YOU
PERSONNEL

Witold Libionka, MD PhD
specialist in neurosurgery and neurotraumatology
Connected with neurosurgery since 1998, when he started his scientific activity and then, remaining a scholarship holder of the Ministry of Health, individual studies at the Department of Neurosurgery and Neurotraumatology of the Jagiellonian University Medical College. He continued his education at PhD studies at the Faculty of Medicine CMUJ in Krakow (2002-2006). During his specialisation in neurosurgery at the Department of Neurosurgery and Neurotraumatology of the Medical University of Krakow (2003-2010) he participated in numerous training courses to improve his professional qualifications (including Poland, USA, Germany, France). He completed a one-year research and clinical fellowship in functional and stereotactic neurosurgery at the Department of Neurosurgery, University of Rochester, USA.
Combining his professional and scientific work, he performs dozens of surgeries per month and participates in numerous research projects. He is the author or co-author of nearly a hundred publications and reports. His work on the mechanisms of action of deep brain stimulation has been awarded at national and international conferences and has been published in Nature Medicine and Nature Neuroscience.
He is an international consultant, teacher and lecturer in functional neurosurgery and oncology using functional mapping. He has expert experience in deep brain stimulation, spinal cord and peripheral nerve stimulation, intrathecal pump-assisted baclofen treatment, and resection of glial brain tumors in the eloquent area performed with intraoperative awakening and electrophysiological monitoring of speech, movement, vision, hearing, and tactile functions (more than a thousand such procedures performed in total).
Anna Włodarczyk, Msc
psychologist, psychotherapist
- psychologist with clinical specialization, sexologist, psychotherapist
- certified instructor of addiction therapy. Graduate of the Warsaw School of Social Sciences and Humanities
- member of the Polish Psychological Association.
- court expert
- a participant of a specialized training for profilers of missing persons
- an expert of the Opole Province Headquarters of the State Fire Service in Opole in the area of widely understood psychological support
- implementer of preventive social campaigns, for which she was awarded the title “Man of the Year 2016 in the plebiscite of NTO”
- member of TSO, since 2006 closely associated with the State Fire Service as a Regional Rescue Specialist, in the field of psychological support for accident victims and firefighters
- trainer in the field of teamwork, team building, contact with victims, including the profiles of missing persons, debriefing and defusing
- handler of two dogs prepared for rescue work (with one she passed the exam of field specialty of class 0 of PSP)
- Psychologist in Vital Medic Hospital in Kluczbork
Professional interests: since the cooperation with the Vital Medic Hospital, neuropsychology comes to the fore (more on this soon) and associated with the love of dogs activity in the Foundation “Opolsar,” the unit specialized in the search for missing persons using rescue dogs.

Mateusz Pawłowski, MD
specialist in neurosurgery
A graduate of the Faculty of Medicine in Zabrze, Silesian Medical University in Katowice. Participant of doctoral studies at the Medical University of Wroclaw. Doctoral student at the Medical University of Wroclaw.
Specializes in neurooncology, spine and hydrocephalus surgery. He has improved his knowledge and skills during numerous national and international courses.

Olga Milczarek, MD PhD
specialist in neurology and pediatric neurology
Adiunkt Kliniki Neurochirurgii Dziecięcej Instytutu Pediatrii Uniwersytetu Jagiellońskiego Collegium Medicum w Krakowie, aktywny pracownik naukowo – dydaktyczny. Ukończyła specjalizację z neurologii w roku 2013. Staż specjalizacyjny z zakresu neurologii dziecięcej zrealizowała w Klinice Neurologii Dzieci i Młodzieży Instytutu Matki i Dziecka w Warszawie, a egzamin specjalizacyjny z zakresu neurologii dziecięcej złożyła w listopadzie 2021. Od wielu lat współpracuje z ośrodkami neurochirurgicznymi w całej Polsce jako neurofizjolog śródoperacyjny. Zajmuje się również neurochirurgią czynnościową (implantowanie stymulatorów nerwu błędnego, leczenie operacyjne padaczki, wykorzystanie głębokiej stymulacji mózgu -DBS). W trakcie zdobywania licencji z zakresu EEG – interpretuje badania dzieci i dorosłych. Autorka i współautorka licznych publikacji w czasopismach o zasięgu krajowym i międzynarodowym z zakresu neurochirurgii, neurologii, neurologii dziecięcej i neuropsychologii. Autorka wielu doniesień zjazdowych z konferencji krajowych i międzynarodowych. W obszarze zainteresowań znajduje się przede wszystkim leczenie padaczki, w tym lekoopornej u dzieci i dorosłych z wykorzystaniem nowoczesnych zdobyczy medycyny, w tym diety ketogennej i CBD, diagnoza zaburzeń rozwoju mowy, zaburzeń zachowania, problemów neurorozowjowych, leczenie skutków encefalopatii, urazów czaszkowo – mózgowych i bólów głowy.
